Oct 9, 2019
Chair’s Column: Where We are Taking Action to Address Unprofessional Behaviour in the Department of Medicine
About Us, Cardiology, Clinical Immunology & Allergy, Clinical Pharmacology & Toxicology, Division of Dermatology, Education, Emergency Medicine, Endocrinology & Metabolism, Faculty, Gastroenterology & Hepatology, General Internal Medicine, Geriatric Medicine, Hematology, Infectious Diseases, Medical Oncology, Nephrology, Neurology, Occupational Medicine, Physical Medicine & Rehabilitation, Quality & Innovation, Research, Respirology, Rheumatology, Palliative Medicine

 In the last issue of DOM Matters
In the last issue of DOM Matters 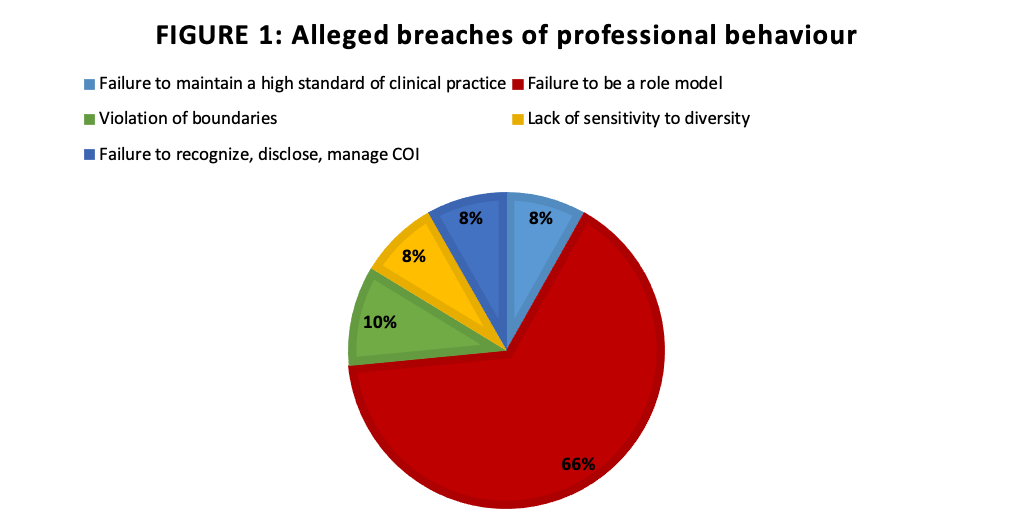 An additional 10% of complaints related to violation of boundaries, and 8% each to failure to maintain a high standard of socially responsible clinical practice, including repeated failure to be available for scheduled duty or teaching, reporting for work when unable to perform required duties and questionable prescribing; lack of sensitivity to and acceptance of diversity; and failure to recognize, disclose, and manage competing interests.
An additional 10% of complaints related to violation of boundaries, and 8% each to failure to maintain a high standard of socially responsible clinical practice, including repeated failure to be available for scheduled duty or teaching, reporting for work when unable to perform required duties and questionable prescribing; lack of sensitivity to and acceptance of diversity; and failure to recognize, disclose, and manage competing interests.

