Chair's Column: Professional Fulfillment and Wellness in the Department of Medicine: Results of the 2019 Faculty Survey

Dr. Gillian Hawker
Thank you for participating in the DoM Survey! We are listening to you and learning from you.

Every other year, we conduct a survey of our faculty members to assess the culture and well-being of our department members here at the University of Toronto and to inform departmental actions. Volunteer faculty members design and pilot test these surveys. In 2017, we asked about career satisfaction and potential determinants. We were pleased to report that career satisfaction was high (88% of female and 84% of male faculty members were somewhat or strongly satisfied), and that the proportion that reported feeling ‘burned out’ from work was modest (64% indicated never or infrequently experiencing feelings of burnout). Following up from this survey, qualitative feedback suggested that enhanced mentorship or coaching, attention to unprofessional behavior and strategies to address increasing clinical volume and complexity have the potential to improve career satisfaction and wellness within our field.
Based on these findings, here in the Department of Medicine, we expanded our mentorship program by appointing divisional Mentorship Facilitators, implemented a mid-point, one-and-a-half-year check-in after initial DoM faculty appointments, and will soon be introducing confidential Retirement Coaches to help mentor late career transitions.
Together with our hospitals, we are investing heavily in leadership development, coaching, and assessment. Professional behavior is an expectation and many of our hospitals and our academic divisions have created methods to recognize exemplary citizenship.
Finally, our hospital and divisional leaders have been pushing to enhance clinical support through recruitment of hospitalists and advanced practice practitioners, and through new models of care.
We are off to a good start, and are beginning to see the impact, but we know that there is more to be done.
The 2019 Survey
Our third biennial faculty survey, conducted this past spring, examined our department’s culture under four themes: Diversity, Work Environment, Physician Wellness and Work Structure. To foster participation as well as honest, constructive feedback, responses were anonymous. In presenting the results, we have excluded results with fewer than six respondents.
Respondent Characteristics
Of our 805 full-time clinical faculty members, 419 completed the 2019 survey (52%). A total of 42% of respondents were female and there was a wide range of age groups, specialties, hospitals, academic position descriptions and ranks. Twelve individuals (3%) self-reported being a person with a disability. 21% described growing up in a family identifying as lower or lower-middle income (15% in 2017). Over half (57%) indicated their race/ethnicity as “White” (60.5% in 2017), while 109 respondents (30%) identified as a person of colour or member of a visible minority. The majority, 93%, identified as a man or a woman (95% in 2017). A total of 64% indicated that they provide care for one or more dependents (56% in 2017).
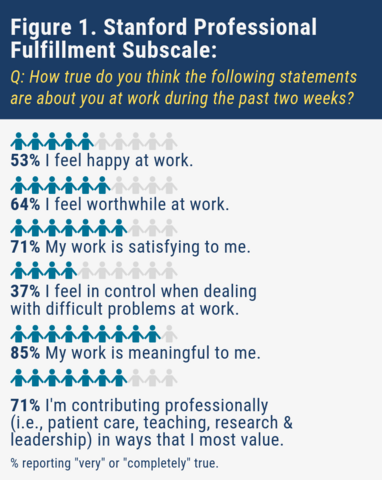
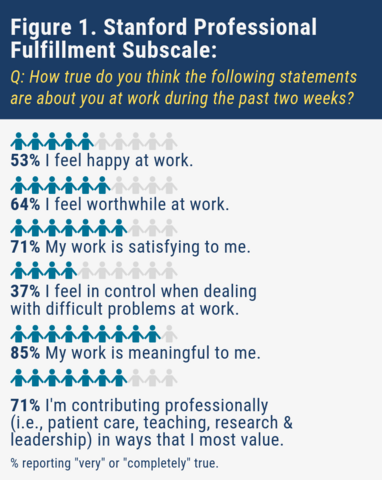
This year, we asked respondents to complete the validated Stanford Professional Fulfillment Index. This measure is composed of three subscales scored from 0 to 10:
- Professional Fulfillment;
- Work Exhaustion and
- Interpersonal Disengagement.
Scores for work exhaustion and interpersonal disengagement are combined to assess burnout. A score of greater than 3.3 out of 10 correlates with a high level of burnout.
2019 Survey Findings:
 A Brief Overview of Survey Results:
A Brief Overview of Survey Results:
- Faculty members find their work meaningful, but perceived that a lack of control when dealing with difficult problems at work is detracting from their overall professional fulfillment.
- Although lower than what is estimated in the United States, 31.8% of our faculty members met the criterion for burnout. The Faculty Survey shows us that symptoms of burnout are higher among women, those with disability and those at earlier stages of their careers.
- There is a strong relationship between professional fulfillment and burnout with work-related factors, including the level of respect and civility among colleagues. This supports our ongoing efforts to address unprofessionalism in the workplace. Analyses are underway to examine the relative contribution of sociodemographic, professional and organizational factors on physician wellness in our department.
- Although faculty are increasingly aware of policies and procedures to address unprofessional behavior, they remain concerned about retaliation in response to taking action.
- 53% of respondents are willing to consider a reduction in total income to improve their well-being. This underscores the need to advance alternate models of care for the aging population and for physicians.
- Over one thousand qualitative comments were provided by faculty survey participants. These data are yet to be fully explored and are expected to further our understanding of our faculty culture and opportunities for the future.
Detailed Findings:
Physician Fulfillment and Burnout
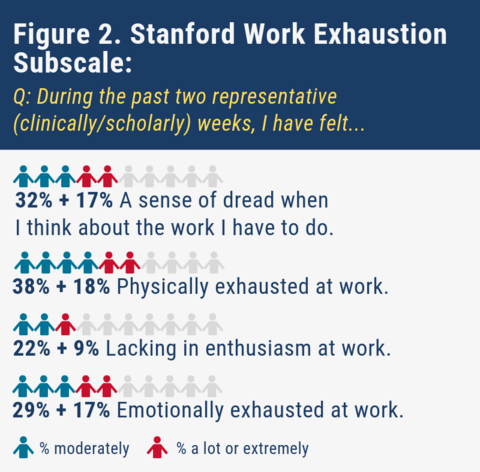
Work Exhaustion Subscale:
The mean score for work exhaustion was 3.5/10 (lower scores are better). More than half of the respondents (56%) reported feeling moderately, a lot, or extremely physically exhausted. Almost half (49%) reported a sense of dread when thinking about the work they have to do, 31% reported lack of enthusiasm at work and 46% reported being emotionally exhausted at work (Figure 2). These rates have caught our attention and re-established our commitment to exploring ways to improve workplace efficiencies in collaboration with our hospital leaders.
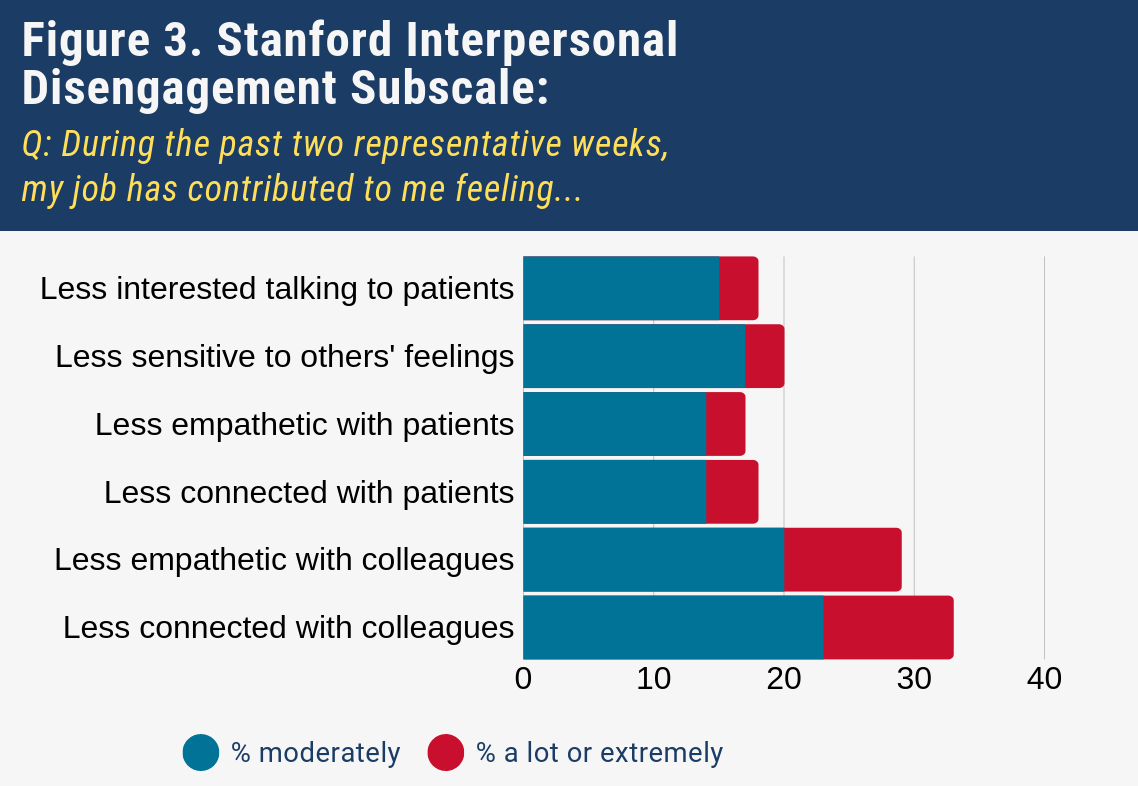
Personal Disengagement Subscale:
The mean score for personal disengagement was 2.1/10 (lower scores better). While less than five percent of faculty respondents felt that work had contributed to disengagement with patients (Figure 3), one in ten indicated that work had contributed a lot or extremely to their feeling less connected to or engaged with colleagues as well.
 Physician Burnout
Physician Burnout
The mean burnout score was 2.8 out 10 (lower scores better); 31.8% of faculty respondents met the criterion for burnout.
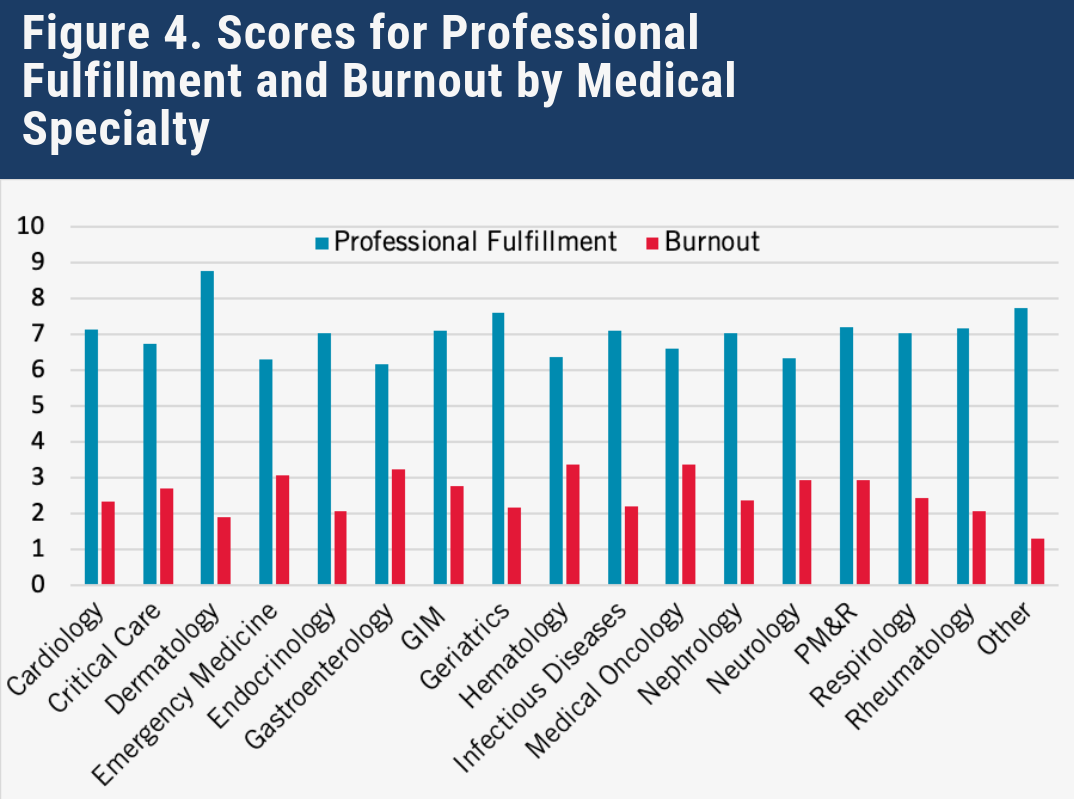
Professional Fulfillment and Burnout by Age Group, Sex, Division, Hospital and Rank
Scores for professional fulfillment and burnout did not differ significantly by medical specialty (Figure 4), hospital, or caregiver status (p>0.05 for all). Individuals at earlier stages of their careers, such as those at a lower academic rank or in a younger age group, and those with majority-clinical position descriptions, reported modestly less professional fulfillment and more symptoms of burnout than those at later career stages and those with majority-scholarship position descriptions.
Mean burnout scores were significantly higher for women than men (41.8% versus 23.5%, respectively [p<0.001]). Women also had significantly lower scores for professional fulfillment (p=0.006). Although the numbers of respondents who reported being a person with a disability was small (12 identified as such), these individuals also reported significantly lower professional fulfillment and higher burnout (p<0.01 for both).
Work Environment
Most respondents agreed that the people they work with interact with them in a respectful and civil manner (82% strongly or somewhat agreed). The mean score for satisfaction with efforts made to create a collegial and supportive environment that promotes inclusivity was 2.6 out of 4, where higher scores indicated greater satisfaction. More than half of our faculty (56.6%) indicated they had witnessed unprofessionalism at work within the past two years and 41.1% reported having experienced unprofessionalism themselves. These current numbers are higher than respondents reported in 2017. Potential explanations include a true increase in unprofessional behaviours, perhaps due to increasing clinical and academic workloads. This could also be the result of surveillance bias, or a heightened awareness or increased willingness to report unprofessional behaviours. Either way, this warrants our attention.
Most of our faculty members are aware of policies and procedures to address unprofessionalism (59% at the university department level and 70% at hospital level), however, only one-fifth were ‘strongly confident’ that they could take action to address unprofessionalism without concern for reprisal.
Relationship of Work Environment to Professional Fulfillment and Symptoms of Burnout
We looked at the relationships between perceptions of the work environment and professional fulfillment and burnout. Perhaps not surprising, professional fulfillment is higher, and burnout lower, among those who perceived their colleagues to be respectful and civil, who are satisfied with institutional efforts to create a supportive and inclusive environment, and who have higher levels of confidence that they could address unprofessional behavior without fear of retaliation (p<0.001 for all).
Work Structure and Work Load
In 2017, our faculty members told us that they were struggling to find the right balance of work with life outside of work. This year, we looked at faculty members’ preferences towards various strategies to manage clinical workload as a means to help with work-life balance.
We found that an overwhelming majority (92%) of respondents are willing to reduce their clinical hours, 73% to reduce their clinical income, 53% to consider a reduction in total income and 69% would consider a salaried position if not already in one.
With respect to how to achieve a reduction in clinical workload, there was substantial variation across divisions, but interest was highest for three responses:
- Recruitment of additional faculty;
- Exploration of alternate funding models and
- Sharing the workload with other types of care providers.
Next Steps:
The 2019 Faculty Survey findings are striking. We want you to know that the department is fully committed to working with our hospital colleagues to enable you to find “joy and meaning” in your work.
At our upcoming departmental strategic planning retreat later this month (September 24 and 25, 2019), the findings of the 2019 Faculty Survey will be presented and discussed, and a plan of action will be developed. Concurrently, the Dean of Medicine and the TAHSN CEOs have already identified wellness as a priority, have struck relevant working groups, and will be holding a joint retreat in November 2019. DoM members are actively engaged in this work, which will be important in informing our own DoM Wellness Strategy.
With the appointment of Dr. Sharon Straus as Physician in Chief at Unity Health Toronto / St. Michael’s Hospital, the Vice Chair, Mentorship, Equity, Diversity (MED) portfolio has become vacant. This has given us the opportunity to consider how best to grow the important work that the MED committee has done during Sharon’s tenure. To reflect the direction that this portfolio has taken, we will be renaming the position as Vice-Chair, Culture and Inclusion. It will have three thematic foci, each with a faculty lead:
- Mentorship;
- Equity, Diversity and Inclusion; and,
- Wellness.
The posting for the Vice-Chair (VC) position will be forthcoming, and the new VC will participate in recruitment of the faculty leads.
We continue to refine our approach to investigating complaints of incivility / unprofessional behavior arising from our learners and faculty members. We are working closely with PGME to align processes and ensure as best we can that people feel safe to bring issues to our attention and that our faculty members feel that processes are fair and transparent. Retaliation remains a real concern for all, which we need to address.
Finally, the survey findings underscore the critical need for a stream of physicians in academic medicine whose primary focus is on delivering high quality clinical care. The pros and cons of varying and diverse strategies are under consideration.
We will follow-up late fall with an update – stay tuned.
Let me close by thanking those of you who took the time to participate in the 2019 Faculty Survey, and specifically to Sharon Straus, Reena Pattani, Karen Burns, Andrea Page, Caroline Chessex, Ed Lorens, Lillian Belknap and other members of the MED Committee for their leadership. As always, I want to hear what you have to say. Please email your comments and thoughts to be at g.hawker@utoronto.ca.