Emergency Medicine: Resident Resources
General Resident Resources
Program Leadership and Contacts
 |
Kaif Pardhan, MD MMEd FRCPC, |
|
 |
Jennifer Chu, MD, MPH, FRCPC, |
|
 |
Tim Dalseg, MD, MPH, FRCPC, |
|
|
VACANT |
|
|
|
 |
Jasmine Xue |
|
 |
Jenn Robertson Department of Medicine |
Contact for:
|
 |
Carolyn Laidlaw Program Coordinator Department of Medicine |
Contact for:
|
|
Hospital Site Contacts UHN: Drs. Ada Gu and James Fairbairn If you do not have a site coordinators contact, please email Jenn at program.em@utoronto.ca. |
||
|
Lead Residents 2023/24 Kate Dillon (PGY3) Hanna Jalali (PGY3)Kara Tastad (PGY3) Rachel Trister (PGY3) |
|
|
|
Junior Resident Representatives 2023/24 |
|
|
|
PGY1 Representative 2023/24 TBD |
|
|
Academic Day
Our program has one full academic day per week (Tuesday). Attendance at the academic day (both morning and afternoons) is mandatory, and must be logged within 24 hours via the attendance survey.
Attendance Policy
Transition to Discipline
New as of July 2018, PGY1 residents will have a dedicated 3 block academic day with tailored sessions – lectures, workshops and simulation. Dr. Rob Simard is the TTD academic lead. Here is a link to the schedule.
Foundation of Discipline
Upon completion of the TTD academic day sessions, the PGY 1 residents will join the rest of the residents at our academic day, with the exception of Foundation Rounds that are only for PGY1s and run every Wednesday from 8:30-10 am. The Foundation Rounds are led by Dr. Rob Simard.
For the remainder of the schedule please link to our Google calendar. We recommend you sync this calendar with your own ical or Google calendar, so changes will be reflected in your own calendars.
Core Academic Days
PGY 2-5’s attend Core Academic Days that consist of morning and afternoon sessions. The morning sessions cover Rosen chapters and a series of other didactic sessions including Grand Rounds. The afternoon sessions consist of small group sessions that cover our longitudinal curricula (see below). Core Academic Days run on a 2 year cycle.
In addition to academic day, residents are required to attend the following mandatory events:
- Critical Skills Day
- Disaster Simulation Day
- Visiting Professor Day
Afternoon Sessions - Longitudinal Curriculum
Full description is found here.
- Journal Club – all years
- Wellness Rounds – all years
- Simulation – all years (note: a separate schedule is sent for simulation so you will know which sessions you need to attend)
- Leadership Rounds – all years
- Advocacy Curriculum - all years
- Clinical Epidemiology and sessions on Foundations of developing a Resident Academic Project – end of PGY 1
- Ethics – PGY 2
- Quality Improvement – PGY 2, 3, 5
- Geriatrics – PGY 3
- Transition to Practice – PGY4/ 5
Please review the calendar of events details to ensure you attend the sessions which apply to your year.
Vacation/ Leave Requests
- Vacation/Professional Leave Request Process
- Vacation Days Available
- Professional Days Available
- Conference Leave Available
- Holiday/Lieu Days
Vacation/ Professional Leave Request Process
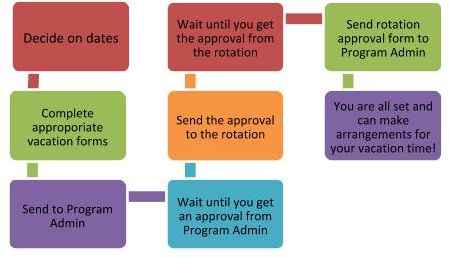 Requests must be made in writing at least 4 weeks in advance of the requested start day of the rotation (recommended at least 6 weeks). Please allow 5-7 business days for the program to process your request. If your request is urgent, please include “URGENT” in the subject line of your email. All vacation and professional leave requests must be approved by the Program Admin first. Leave requests that are not approved by the Program Admin cannot be submitted to the rotations. Each rotation has their own rules regarding submitting vacation requests; please consult with the Program Admin or the rotation for details.
Requests must be made in writing at least 4 weeks in advance of the requested start day of the rotation (recommended at least 6 weeks). Please allow 5-7 business days for the program to process your request. If your request is urgent, please include “URGENT” in the subject line of your email. All vacation and professional leave requests must be approved by the Program Admin first. Leave requests that are not approved by the Program Admin cannot be submitted to the rotations. Each rotation has their own rules regarding submitting vacation requests; please consult with the Program Admin or the rotation for details.All requests must be confirmed or alternate times agreed to within 2 weeks of the request. Rejections must be in writing with the reason for denial. There can be no blanket policies restricting the amount of vacation in any rotation.
Our emergency program requires that you submit a leave request form for all leave requests (vacation, professional days, etc.). There are several forms, choose the appropriate form.
- Vacation, Professional days, Lieu days, Float Days Request Standard Form (updated April 28, 2023)
- Neuro, IM, MC, CCU etc. Vacation/Leave Form (updated June 2023)
- ICU Vacation/Leave Form (updated June 2023)
- Additional Professional Day Request Form for Conference Attendance (updated July 2022)
These requests must be initially approved by the program office and then subsequently submitted to the respective rotation.
You are responsible for the submission to both the program and to the rotation. Once the form has been completely approved, you are responsible for submitting it back to the program office. When planning your vacation, please consider mandatory program events, during which you may not be granted vacation (example include examinations, our annual research day etc.).
Vacation Days Available
4 weeks (a week is 7 days which includes 5 working days and 2 weekend days) of paid vacation per year (no carry-over).
- Vacation, Professional days, Lieu days, Float Days Request Standard Form (updated April 28, 2022)
- Neuro, IM, MC, etc. Vacation/Leave Form (updated June 2023)
- ICU Vacation/Leave Form (updated June 2023)
Professional Days Available
Maximum of 7 working days per year (note: weekends are not considered “working days” for this purpose). You DO NOT need to be attending a seminar or course to take them. Unlike vacation days, you can break up these 7 days into individual days to be taken separately.
- Vacation, Professional days, Lieu days, Float Days Request Standard Form (updated June 2023)
- Neuro, IM, MC etc. Vacation/Leave Form (updated June 2023)
- ICU Vacation/Leave Form (updated June 2023)
Conference Leave Available
As of July 1, 2018, if a resident is going to present their academic work at more than one program-approved conference (which requires travel) in one academic year, they can be given three additional professional days for each additional conference (up to two additional conferences) per academic year. If they present at one conference, there are no additional professional days given. In order to submit a request for 3 additional professional days to present your academic work, please submit “Additional Professional Day Leave Request Form” to the program for approval.
- Additional Professional Day Request Form for Conference Attendance (updated July 2022)
Holiday & Lieu Days
All house staff are entitled to the following recognized holidays:
- New Year’s Day
- Family Day
- Easter Friday
- Victoria Day
- Canada Day
- August Civic Holiday
- Labour Day
- Thanksgiving Day
- Christmas Day
- Boxing Day
- One Floating Holiday (to be picked by the resident)
All house staff are entitled to 5 consecutive days off during the 12-day period encompassing Christmas Day and New Year’s Day. These 5 days account for Christmas Day, New Year’s Day, Boxing Day, and two weekend days. Each resident must get either Christmas or New Year’s Day off.
Lieu Days are granted for residents who are scheduled to work on any recognized stat holiday (or any part thereof, including being on call the day before). Lieu Days must be taken at a mutually agreeable time within 90 days of the holiday worked. No lieu days for Christmas Day, New Year’s Day, or Boxing Day (this is included in the 5 days off over the holiday period).
Lieu days may not be used for a 1:1 shift reduction on shift-based rotations. Lieu days, in combination with professional days, may be used for shift reductions as follows*:
- 1 day = No Shift Reduction
- 2/3 days = 1 shift
- 4 days = 2 shifts
- 5 days = 3 shifts
- 6/7 days = 4 shifts
* Note: This is not based on the collective agreement, but was agreed upon by both PARO and EMRTC.
Religious Holidays
If you observe religious holidays that are not specifically listed in the PARO-CAHO Collective Agreement, your program may have a duty to accommodate your religious practice to the point of undue hardship (“undue hardship” may include a number of factors, such as patient safety, the hospital’s service requirements, and the resident’s educational/training requirements).
It is your responsibility to request an accommodation with a reasonable amount of notice, explain what measures of accommodation are required, and allow a reasonable time for a reply. Since each request is unique, religious accommodation is typically worked out on a case-by-case basis. In some cases, it may be possible to switch statutory holidays listed in the Agreement for your religious holiday. Residents and programs are usually able to come to a mutually agreeable solution once needs are discussed/clarified.
Postgraduate Medical Education Office (PGME) Resources
- PGME Orientation Manual
- Office of Learner Affairs
- Payroll
- PGCorED
- PGME Global Health
- Awards and Scholarships
PGME Orientation Manual
Postgraduate medical education office (PGME) at the University of Toronto, also, provides a PGME Orientation Manual
PGME Resident Wellness
University of Toronto PGME Resources
Please see the Guidelines for Managing Disclosure of Learner Mistreatment here and a website outlining details of raising concerns here. To disclose, discuss or report mistreatment, you may fill out the form on the website or connect with a designated leader.
Office of Learner Affairs (OLA)
Email: ola.reception@utoronto.ca
Website: https://meded.temertymedicine.utoronto.ca/contact-us
Services Offered:
- Confidential counseling/psychotherapy and wellness coaching
- Support during remediation/academic difficulty
- Career and postgraduate training guidance
- Disability and accommodation support
- Educational programming/workshops on themes related to wellness & performance
- Research pertaining to resident wellness
- Contact information to the U of T community
Payroll
The Toronto Hospitals’ Postgraduate Payroll Association (THPPA) is the University of Toronto Faculty of Medicine paymaster for most postgraduate medical residents. Information related to salary, call stipends, benefits, insurance, and taxes for new and returning residents can be found on the PGME website.
PGCorED
The University of Toronto Postgraduate Medical Education PGCorED is a series of self-directed multimedia web-based learning modules which covers the foundational competencies for University of Toronto postgraduate trainees. PGCorEd covers topics in the CanMEDS 2015 Physician Competency Framework and is accessible from any mobile device.
New modules in this series will be made available to PGY1 and 2 residents as they are developed. Residents are responsible to complete their PGCorEd modules before the end of their PGY2 year. Check with your Program Director to confirm if there is a program specific sequence or deadlines for module completion.
PGME Global Health
PGME Global Health is committed to being an international leader in the development of and offering coordinated, inter-specialty global health programming and initiatives. PGME’s Global Health initiatives reflect local and global social responsibility and accountability, supporting PGME trainees towards contribution and leadership in global health education, research and practice. Residents in our Emergency Program have the opportunity to take an elective as part of our Toronto Addis Ababa Academic Collaboration – Emergency Medicine (TAAAC- EM) program.
Supports/Mentorship
At the University of Toronto, Division of Emergency Medicine we have multiple forms of mentorship:
Junior Mentor
This is a current PGY-1 who will be a PGY-2 when you start. Each new PGY 1 will be assigned one junior mentor. These residents are in a unique position to assist new residents with their move to Toronto and can answer questions regarding getting situated, registering with the University, transportation, and resident events. This is an invaluable resource.
One-on-One Staff Mentor
Residents get to choose one of the staff FRCP emergency medicine doctors to be their residency mentor. This mentor is responsible for providing career advice as they advance through your training, and for advocating on their behalf should they get into trouble. Generally, a staff member can mentor more than one resident. Most residents choose a staff member with similar career/personal interests. The choice of staff member should be made by the end of your PGY-1 year. Notify your program administrator of who your mentor is. If you need assistance finding a mentor, contact your program Administrator or Assistant Program Director.
Buddy Groups
Each resident can choose to be assigned to a group consisting of residents from each year, as well as up to three faculty from across the division of emergency medicine. PGY2s in each group are responsible for organizing group activities over the year.
Research Supervisor
Your research supervisor (also called a research mentor) is someone with whom you choose to undertake scholarly activities. This person is usually not the staff person you chose to be your Staff Mentor. Dr. Jennifer Chu and the Resident Academic Project (RAP) committee can help you find an appropriate Research Supervisor. In the fall of PGY-1, you will be asked to submit your research background and interests to Dr. Chu, so the RAP committee can make useful suggestions for whom might make a good Research Supervisor for each of you.
Do not be afraid to approach different staff persons to be your informal mentors/sound boards. We’re all here to help! If you need help connecting with Faculty or Resident mentors email the Program Administrator
Scholarly Activities
 |
| Jennifer Chu |
On behalf of the Resident Academic Project (RAP) committee, it is our hope that this will serve as a comprehensive resource for guiding the generation, development, implementation, and dissemination of high-quality scholarly projects. Here you will find a detailed guide on developing a scholarly project, information on project supervisors, resources for research ethics, and project guides and timelines. We will also provide updates on scholarly events such as the annual visiting professor, and academic day.
Perhaps most importantly, contact information for our stellar RAP committee members. As a group we are all committed to your success as young investigators – so please be in touch!
- Resident Academic Project (RAP) Committee Contacts and Bio
- Research Ethics Board (REB) FAQs
- Cycle and Timeline
- Developing Scholarly Project
- Important Forms to Submit
- Site Specific Research Associates
- Resident Research Funding and Statistical Support Opportunities
- Predatory Journal Checklist
- Clinical Epidemiology
- Research Academic Day Program 2018
EM Residency Training Committee (EMRTC)
Full copy of EMRTC Terms of Reference
Mandate
The purpose of the Emergency Medicine Residency Training Committee (EMRTC) is the implementation and maintenance of the Royal College of Physicians and Surgeons of Canada (RCPSC) Emergency Medicine Specialty Training Program in accordance with the General and Specialty Specific Objectives, Training Requirements and Standards of Accreditation outlined by the RCPSC.
Responsibilities
- To maintain a workable yet detailed set of Program and Rotation-Specific educational objectives that encompass personal and professional attributes and attitudes, clinical skills, technical procedures, and knowledge pertinent to the practice of the specialty of Emergency Medicine.
- To ensure that the structure and operation of the Residency Program enable residents to achieve these educational objectives.
- To consider on a regular basis the results of: o Exceptional ITER's o Exceptional semi-annual evaluations o Exceptional FITERs o Exceptional performance on in-training assessments
- To ensure that the residents are kept informed of their evaluations.
- To maintain an appeal mechanism.
- To establish and oversee a mechanism for career planning and counseling.
- To consider on a regular basis the results of exceptional rotation and teacher evaluations
- To undertake a regular overall program review
- To establish criteria for assessing applications to the program, solicit applications, interview applicants, and decide upon a rank order list of applicants
- To discuss residents not meeting standards of the program, and to make recommendations for coaching/remediation including referral to the University of Toronto Board of Examiners
- To oversee implementation of programmatic curricular and assessment changes (including Competence by Design implementation strategies)
Membership
The EMRTC will be composed of:
- Program Director- Dr. K. Pardhan (chair)
- Assistant Program Director- Dr. J. Chu
- Hospital Coordinators
- St. Michael’s Hospital - Drs. R. Poley and M. Chacko
- Sunnybrook Health Sciences Centre - Drs. A. Stefan and R. Simard
- University Health Network- Drs. A. Gu and J. Fairbairn
- The Hospital for Sick Children- Dr. Natasha Collia
- North York General Hospital - Dr. M. Lipkus
- Member at Large- TBD
- Resident Academic Project Sub Committee Chair - Dr. J. Chu
- Chief Resident(s) (PGY3)- Annually elected
- Junior Representative (PGY2) - Annually elected
- PGY 1 Resident Representative- Annually elected
- Ex Officio Members:
- Division Director- Dr. E. O'Connor
- Program Director CCFP-EM- Dr. A. Chin
- Department Directors
- St. Michael’s Hospital- Dr. C. Snider
- Sunnybrook Health Sciences Centre- Dr. A. Verma
- University Health Network- Dr. S. Sabbah
- The Hospital for Sick Children- Dr. J. Fischer
- North York General Hospital- Dr. K. Wasko
Educational Funding/Reimbursement
Resident Academic Funds
There will be $750/year for use towards academically related purchases. For example, these funds may be used to build your emergency medicine library or to attend conferences (travel, conference fees, etc.). This also includes medical software purchases for your PDA/Smartphone but not for the purchase of hardware. You must keep receipts of your purchases and fill out a reimbursement sheet.
Terms of Academic Reimbursements
- Up to 750 per academic year. Academic funds do not carry over at the end of the academic year. Must be submitted by June 30th. If you need to check if you have funds left check with division.em@utoronto.ca
- Academic Reimbursements apply for educational books; software or apps; conferences in which you are not presenting; travel/accommodation for rotations outside of Toronto; certificate courses/educational courses;
- DOES NOT INCLUDE: laptops; iPads; any hardware purchases; items unrelated to residency education
- If not listed please contact division.em@utoronto.ca to see if it will be approved.
Steps to applying for Academic Reimbursement
- Fill out the Academic Reimbursement Form
- Submit the appropriate supporting documents & original receipts
- The DOM wants original receipts not scans. You can drop them off to me at the DOM. The DOM’s address is located at TGH. It’s 6 Queen's Park Crescet West, C. David Naylor Building, Third Floor. You can either leave it with the Admin at the front or bring it back to me in the office. The office has staff at the front from 9am-5pm
- Supporting Documents/ Receipts (DOM Requirments)
- Digital Receipts- The DOM wants original receipts. If the digital receipt you have is the original that was sent to you. Make a note that is the original copy or send me an email stating it is the original copy. That way we do not have to follow-up with you or the conference/course to find out what type of receipts they provide
- Cash payments- If you paid for something in cash, please note it so we don’t ask for a credit card statement
- Items purchased by Credit Card- if you purchased something by credit card, please include a copy of the statement. Especially if the receipt or statement doesn’t show payment was made and received or how it was paid for.
- Conferences/Courses- You are not able to submit before attending. The DOM wants certificates of attendance or something that confirms you attended. If the Conference/Course does not provide certificates, send the division admin an email stating you attended the conference/course and they do not provide certificates. This will be the additional documentation the DOM will use.
- Someone else bought it for you and you paid them back- Send an email clearly explaining the circumstances when submitting documents. If possible, always pay for whatever you are asking for reimbursement yourselves.
- Split reimbursement- If you and another resident are splitting a reimbursement (eg shared accommodation while on Tox rotation in New York) again send a clear email explaining the split purchases.
- Travel and Accommodation for Rotations outside of Toronto- please include the name of the rotation, dates of rotation, and supervisor while on rotation.
- Supporting Documents/ Receipts (DOM Requirments)
- The DOM wants original receipts not scans. You can drop them off to me at the DOM. The DOM’s address is located at TGH. It’s 6 Queen's Park Crescet West, C. David Naylor Building, Third Floor. You can either leave it with the Admin at the front or bring it back to me in the office. The office has staff at the front from 9am-5pm
Resident Conference Award
To encourage residents to prepare and present scientific abstracts at national and international conferences, the Division of Emergency Medicine is providing limited financial support to residents whose work has been accepted for presentation.
Terms of Conference Award
- Max one conference submission per year up to $1000 per resident. Funds do not carry over at the end of the academic year. Must be submitted by June 30th, with conference completed in that academic year. If you need to check if you have funds left check with division.em@utoronto.ca
- Resident must be physically present at the conference to receive funding and have proof of attendance.
- The program director reserves the right to decline to provide funding to a resident who will present at a conference determined to be of low academic value or relevance (the resident may appeal this decision to the EMRTC)
- Poster Presentation: $750
- No difference for moderated or not moderated
- “e-poster” (poster without paper): same value as a traditional poster
- Oral presentation: $1000
- Pre-recorded presentation (e.g. at SMACC): same value as an oral presentation
Steps to applying for Conference Award
- Fill out the Conference Award Form
- When filling out the form, make sure to add your Date of Birth and SIN number for payroll purposes. This is an award and must be noted on your taxes. This will be on your T4A in box 28 as an award.
- Submit the appropriate supporting documents
- Residents must provide copies of the letter of acceptance of the abstract(s) following conference peer-review, a copy of the abstract(s), and a conference program confirming the presentation to be eligible for support. Must submit originals, not scans. Receipts are not needed to be submitted. This is a scholarship and must be noted on your taxes. You can drop them off to the Division Administrator at the DOM. The DOM’s address is located at TGH. It’s 6 Queen's Park Crescet West, C. David Naylor Building, Third Floor. You can either leave it with the Admin at the front or bring it back to me in the office. The office has staff at the front from 9am-5pm.
- DO NOT SUBMIT RECEIPTS FOR THIS AS IT WILL BE CONFUSED FOR ACADEMIC REIMBURSEMENTS
Policies/Protocols
Resident Attendance at Academic Day Policy
As adult learners, residents are allowed to miss an academic day for any reason they deem appropriate (including post call, illness, family or personal emergency, balancing wellness, etc.). However, there is a set proportion of days you can be absent. This limit has been set at 20% absences of all mandatory events (with a few exemptions - see the full policy for details). Vacation is exempt in addition to this 20% allowance. If you are going to miss any small group session (all afternoon sessions have 10 or fewer people scheduled to attend), please notify the instructor and the Program Admin as soon as possible so they can plan accordingly.
Please review the full Resident Attendance at Academic Day Policy for additional details (updated August 2023)
Clinical Duty Scheduling and Absenteeism Policy
This policy is intended to describe the rights and responsibilities of residents within the FRCP Emergency Medicine residency training program with respect to scheduling and attending clinical duties during rotations. This policy is to be used in addition to PARO scheduling guidelines. In the case of discrepancies, the most updated PARO guidelines will supersede this policy.
Please review the full Clinical Duty Scheduling and Absenteeism Policy for additional details (updated August 2023)
PGY 4 / 5 Work-Life Balance Policy
EMRTC recognizes that there are two important considerations for the PGY4/5 years:
- To transition PGY 5residents to practice as high-quality emergency medicine consultants
- To prepare for success at the Royal College Emergency Medicine Examination
Please review the full PGY4 Work-Life Balance Policy for additional details (updated August 2023)
Protocol for Unsatisfactory Resident Performance
This policy is intended to describe the process to be followed in the case of unsatisfactory resident performance in the FRCP Emergency Medicine Program. The program adheres to the Guidelines for Assessment of Postgraduate Residents of the Faculty of Medicine at the University of Toronto
Resident Safety Policy
This policy provides background to the relationship between the University and all Clinical teaching sites with respect to resident safety.
- Resident Safety Policy (updated August 2023).
Postgraduate Medical Education (PGME) Office Policies and Guidelines
Department of Medicine (DOM) Policies
Restricted Registration
Are you considering applying for a Restricted Registration License?
Our program has participated in the Restricted Registration program (RR) for a number of years. RR brings many benefits for the residents, and we are happy to support our resident’s involvement in it. Please be advised that obtaining an RR license is a privilege and not guaranteed to all residents. Assessment of resident eligibility to apply for an RR license and approval of the application is at the discretion of the Program Director in consultation with the Competence Committee and EMRTC, and is decided on an individual basis. Our residents are allowed to obtain an RR license in PGY 3-4 in the non-CBD cohort and in PGY 3 (and potentially PGY 5 – subject to change) in the CBD cohort, and are expected to follow the steps outlined below:
- Before starting your application process, please review the requirements on the CPSO and RR website in detail. You are responsible for all steps in the process and complying with the conditions of the RR license.
- Approval will have to be obtained at regularly scheduled Competence Committee meetings.
- Ensure that the RR work does not interfere with the clinical and non-clinical work requirements of the residency program. For example it is not acceptable: to miss academic day, show up late or miss program related shifts, miss mandatory program events etc. to work under a RR license.
- Ensure that any additional hours worked not be done in a fashion which would contravene the PARO-CAHO collective agreement. You are responsible for your wellness and maintaining patient safety standards.
- The Competence Committee reviews your file on a regular basis. Should you fail to maintain academic standing or fail to comply with the above, you will be asked to cease working under the RR license. In the situation were there is non-compliance, the Program Director will notify the RR Program office and the Postgraduate Dean of these concerns and recommend cessation of the RR license. This will be effective immediately and there can be no appeal of this decision. Please be advised that a RR license is a CPSO license, and termination of the RR license will significantly impact your future CPSO licensing applications.
PARO Contract
The purpose of the PARO contract is to provide an orderly employment relationship between Ontario teaching hospitals as represented by the Council of Academic Hospitals of Ontario, hereinafter CAHO, and the residents in these teaching hospitals represented by the Professional Association of Residents of Ontario, hereinafter PARO, in order to facilitate the relationship between residents and hospitals so that housestaff will be reasonably compensated for the duties which they perform as hospital employees, and at the same time be able to take advantage of the training program which each individual housestaff enjoys.
Memberships, Conferences, & Medical Courses
Organizations:
- CAEP - Canadian Association of Emergency Physicians (includes a subscription to the Journal of Emergency Medicine)
- ACEP - American College of Emergency Physicians (includes a subscription to Annals of Emergency Medicine)
- EMRA - Emergency Medicine Residents Association (includes a subscription to Annals of Emergency Medicine)
- TAC - Trauma Association of Canada (includes a subscription to Journal of Trauma)
- OMA/CMA - Ontario Medical Association/Canadian Medical Association (includes a subscription to the CMAJ)
- SAEM - Society of Academic Emergency Medicine (includes a subscription to Academic Emergency Medicine)
Conferences:
Residents who present either oral or poster presentations at conferences national or international conferences can apply for the Resident Conference Scholarship (found in the Educational Funding/Reimbursement dropdown under General Resident Resources)
Toronto (local)
- North York General (www.emupdate.ca)
- University Health Network (www.uhn.on.ca/emergencyconference.asp)
- Sick Kids' Pediatric Emergency Medicine Conference (www.sickkids.ca)
National
- Trauma Association of Canada Annual Scientific Meeting (www.traumacanada.org)
- Canadian Association of Emergency Physicians (www.caep.ca)
- Canadian Critical Care Conference (www.canadiancriticalcare.ca)
- Society of Toxicology of Canada Annual Symposium (www.stcweb.ca)
- Canadian Conference on International Health (www.csih.org/)
International
- International Conference on Emergency Medicine (icem2023.com)
- Emergency Medicine in the Developing World (www.emssa.org.za)
- Rocky Mountain Trauma and Emergency Medicine Conference (https://www.traumacenters.org)
Medical Courses
There are several extra courses that you should be aware of:
- BLS/ACLS Provider: This is a must for emergency residents. As a first-year resident, this course is paid for by PGME. Several of the hospitals offer these courses year-round. If you are interested in attending these courses at Sunnybrook, you can contact Sandhya D'Souza at sandhya.dsouza@sunnybrook.ca. Alternatively, you can find all of the courses offered nationally on any given date by logging on to the heart and stroke foundation website.
- ACLS Instructor: This is a useful course if you plan to join the growing number of emergency residents teaching ACLS! Teaching ACLS not only is a good way to make money but it also dramatically improves your cardiac arrest skills. Contact Sandhya D'Souza or the Heart and Stroke Foundation
- ATLS: This course is a useful introduction to trauma care. It is not essential to take this course as most of the material will be covered in Group A lectures. However, it does serve as a good introduction to trauma and would be most valuable if taken before doing your trauma rotation. If you plan on moonlighting as a senior, keep in mind that many of the hospitals do require this certification. Contact Sandhya D'Souza for more information.
- PALS: Sunnybrook has just started to run a PALS course four times annually. Sandhya D'Souza will have more information if you’re interested. During your pediatrics rotation at North York General Hospital (NYGH), you will receive an hour overview of the PALS guidelines. NYGH also offers a Neonatal Resuscitation Course that is valuable to take prior to starting your Pediatric rotation there.
CBD Residents
PD Message
 |
 |
Welcome to the University of Toronto, Emergency Medicine Residency Training Program! This Royal College of Physicians and Surgeons of Canada (RCPSC) postgraduate program is the one of the largest in the country and is situated in a world-class city. With endless arts and music festivals, unparalleled multiculturalism, and mouth-watering culinary delights, Toronto has attracted physicians from across the globe to its eclectic neighborhoods. Whether you’re a fashionista or a foodie, if you’re into sports or spas, if you love reading or rock-climbing, Toronto is the city for you.
Training in a city like Toronto will expose you to people from all walks of life, with a broad range of ethnicities, socio-economic backgrounds, and medical needs. These diverse experiences will be instrumental in your education as a clinical expert and will also foster growth as a patient advocate. Our faculty and residents are as diverse as the Canadian population they serve; they bring an exciting palette of colour to our program with their gamut of interests and expertise. These internationally-known leaders will become your mentors, colleagues, and friends when you join our emergency medicine community.
We are excited to offer a variety of training sites within the city including tertiary care emergency departments, two trauma centres, the pediatric emergency department at the Hospital for Sick Children, and multiple opportunities to work in community emergency departments.
Residents attend weekly full day “Academic Days” and are excused from their clinical responsibilities to do so. Activities on this day are led by both faculty and residents and include interactive case-based seminars, formal didactic rounds, procedural workshops, journal clubs, and team-based simulation sessions. Formal courses are also provided in clinical epidemiology (PGY-1), ethics (PGY-2), geriatrics (PGY-3), quality improvement and patient safety (longitudinal), and a dedicated transition to practice curriculum (PGY-4 and 5). PGY-1 residents have a dedicated ultrasound rotation that leads to Canadian Emergency Ultrasound (CEUS) certification, and there is ample opportunity to pursue further ultrasound training in more senior years and with a core rotation in advanced emergency department ultrasonography.
We are also delighted to be able to offer a full year in PGY-5 to pursue an Area of Advanced Learning (AAL). During this year, each resident can pursue a personally designed curriculum (requires program approval) with the goal of developing expertise in an area relevant to emergency medicine. In the past, areas of focus have included: pediatric emergency medicine; Master of Clinical Epidemiology; Master of Medical Education; Master in Health Administration; Master of Public Health; inner city health; international health; toxicology; trauma; critical care medicine; sports medicine; prehospital care; medical informatics; research; aeromedical transport; clinician-scientist program; bioethics; international emergency medicine; ultrasound; simulation; geriatric emergency medicine and journalism.
That’s our amazing program in a nutshell! If you have further questions, do not hesitate to contact us. If you happen to be in Toronto and want to meet with us, please contact our program coordinator (below) to schedule a meeting or drop by at our academic day
Kaif Pardhan, Program Director
Jenny Chu, Assistant Program Director
PGY1 Orientation Manual
Here is a printable copy of the PGY1 CBD Orientation Manual. This manual includes the residency program policies and processes. For CBD related items see below.
Introduction to CBD
What is CBD?
-
Competence by Design (CBD) is a Royal College of Physicians and Surgeons of Canada (RCPSC) initiative to transition postgraduate medical education and professional practice in Canada into a model of competency-based medical education.
What does that mean to you? There is a shift towards a coaching model of training in lieu of the current performance model. In the coaching model, you will be required to complete formative assessments called Entrustable Professional Activities (EPAs). EPAs are tasks of the discipline that can be delegated to a resident and observed by a supervisor. Typically, each EPA integrates multiple abilities simultaneously (milestones) when performing professional activities (e.g. we use our medical expertise, but also our communication skills). You will learn more on EPAs in the Assessment Section. Here is a link to a CBD Terminology Page for more information
Feedback
- Moving towards a coaching model will entail being able to receive feedback. Feedback can trigger negative reactions on the part of the receiver if it is perceived as a judgment on personal worthiness. Take a look at this Infographic and reflect on how you perceive yourself. We strongly recommend that you also read “Thanks for the Feedback” by Douglas Stone and Sheila Heen before you start residency and that you continue to refer back to it during your career.
CBD Stages
- Residency will continue being 5 years. It will be split into 4 stages:
-
- Transition to Discipline (TTD) 3 Months in PGY 1
- Foundations of Discipline (FOD) 9 Months in PGY 1
- Core of Discipline (COD) 3 years PGY 2-PGY4
- Transition to Practice (TTP) 1 year PGY 5
- The Royal College Exam will take place after the Core stage at the end of PGY 4 (instead of at the end of residency). The RCPSC will be providing more information in the coming years.
CBD champions
- Our program has been working hard with multiple stakeholders in the past 2 years to prepare for this transition. We realize that this is a time of change for you, and are here to support you. We will be meeting with you as a cohort on a regular basis to monitor progress. You will also have at your disposal our CBD champions at the different sites (more information will be provided at your orientation session).
Assessments: General Documents
Stage Specific CBD Resident Expectations
As part of CBD residents will be required to complete regular assessments. Here is a link to an overall map of the assessment requirements for all stages.
Entrustable Professional Activities and Special Assessments
EPAs are one component of the assessments and a CBD requirement. Each stage has specific EPAs that are assigned to it (determined by the Royal College Emergency Medicine Specialty Committee), and successful completion at each stage (as determined by Competence Committee) will be required to move from one stage to another. Here is a link to a list of EPAs.Here is a link to the Royal College document for a detailed breakdown. To avoid getting overwhelmed, start by reviewing the first stage (TTD) EPAs (there are only 4!)
- Elentra user guide
- Entrustment Scale
-
The staff physicians who supervise residents during clinical rotations assess EPAs using the Entrustment Scale. We expect that most of the resident EPAs will be given an “Intervention”, “Direction” and “Supervision” category, and only a few will be given “Autonomous” and “Excellence” especially in the early phase of a stage, and in early years of residency.
Special Assessments are non-EPA assessments that are requirements of the Royal College. Each tool is different, and residents will be provided detailed information on their completion under each stage.
Other assessments are called “Notes to File” and “Professional Behavioural Monitoring Form”.
All these assessments will be completed on the Elentra e-platform, and can be initiated by the resident or their supervisor. In general, we expect that each resident complete at least 1 EPA (or SA tool if applicable) per shift on EM rotations and that as the resident is able, they complete EPAs on off-service rotations.
-
- Emergency Medicine EPAs – All Stages
- For more details on stage-specific EPA and SA tool completion please refer to the specific sections below – TTP documents will be provided and uploaded to the website at a later date
In-Training Exams
You are required to attend mock orals and written exams as outlined in the Stage Specific CBD Resident Expectations.
Royal College
TTD Stage Assessments
The Royal College requires that residents complete the assessment requirements for 3 EPAs (TTD 1-3) and one special assessment (TTD SA 1) in Transition to Discipline (TTD). For a detailed guideline please refer to the below links
EPAs
SA
OSCE
TTD residents will also be required to complete an Objective Structured Clinical Examination (OSCE) in TTD, based on the TTD EPAs (scheduled in Block 4).
ITARS - See Below
FOD Stage Assessments
The Royal College requires residents to complete the assessment requirements for 4 EPAs (FOD 1-4) and one special assessment (FOD SA 1) in Foundations (FOD). However, in our program residents are required to complete FOD SA 1 in the Core stage. You will also be required to complete Core EPA 14 requirements in FOD. For detailed guidelines on completing these assessments, please refer to the link below:
EPAs
ITARS - See Below
COD Stage Assessments
The Royal College requires residents to complete the assessment requirements for 15 EPAs (COD 1-15) and five special assessments (COD SA 1-5) in Core (COD). However, in our program, residents are required to complete 14 Core EPAs (COD 1-13, and 15). You are also required to complete FOD SA 1 in the Core stage You will also be able to complete FOD EPA 4 in the Core stage. For detailed guidelines on completing these assessments, please refer to the link below:
EPAs
SA
ITARS - See Below
ITARs
ITARS
ITARs, or In-Training Assessment Requirement, are evaluations that your preceptor or rotation coordinator will complete at the end of each rotation. All ITARs are reviewed by the Competence Committee and the PD, and your previous EM rotation ITARs will also be reviewed by the resident's upcoming EM rotation coordinators to help identify areas to coach them on.
Rotations
- CBD Sample Rotation Schedule
- Transition to Discipline/Foundations
- Core/Transition to Practice
- Area of Advanced Learning
We have made a number of changes to our rotation schedule to align with CBD and also to address some identified gaps. For example, residents will be doing more EM rotations in your PGY 1 year under CBD then our previous rotation schedules.
CBD Sample Rotation Schedule
Here is a link to the Master Rotation Schedule for all 5 years. There are 13 rotation blocks in each academic year. A number of rotations are “on service” (i.e. emergency medicine or related rotations such as EMS and Ultrasound), and some are “off service”. Residents will rotate through our core teaching sites, as well as affiliated sites.
- Core sites:
- Sunnybrook Health Sciences Centre (SHSC)
- St. Michael’s Hospital (SMH)
- University Health Network (UHN): includes Toronto General Hospital (TGH) and Toronto Western Hospital (TWH)
- Affiliated Sites:
- North York General Hospital (NYGH)
- Hospital for Sick Children (HSC)
Transition to Discipline/ Foundations
TTD entails the first 3 blocks of the CBD PGY 1 year, and FOD the remaining 9 blocks. Here is a link to a Sample Learner Schedule for TTD and FOD. Residents will each be provided their own specific TTD and FOD learner schedule by email.
In TTD residents do 3 blocks of Emergency Medicine (EM) at one of our core sites (SHSC, SMH, or UHN). In FOD you do 4 months of adult EM (3 at our core sites and 1 at NYGH), 1 Pediatric EM at the Hospital for Sick Children, Ultrasound (includes EM shifts), Sports Medicine, GIM-Clinical Teaching Unit (CTU), Pediatric-CTU and Anesthesia.
Each Rotation has a specific Rotation Plan. Residents should review the Rotation Plans prior to the start of each rotation.
- TTD EM Rotation Plan
- FOD Ultrasound Rotation Plan
- FOD Sports Medicine/MSK Rotation Plan
- FOD Peds CTU Rotation Plan
- FOD PEM Rotation Plan
- FOD Anesthesia
- FOD CTU GIM
For all EM rotations, we have asked that our site coordinators schedule 30% of a resident's shifts with a preceptor. We ask that the resident contact their preceptor and meet them at the start of their rotation, mid-way and at the end of their rotation to discuss objectives and progress. Please be advised that this is a mandatory program requirement. (Clinical Duty Scheduling and Absenteeism Policy)
Core and Transition to Practice
COD entails the full 39 blocks during the PGY2 to PGY4 years. Here is a link to a Sample Learner Schedule for COD. Residents will each be provided their own specific COD learner schedule by email.
In COD, residents do 3 - 5 blocks of Emergency Medicine (EM) at our core sites, 1 in ICU, 2 in Trauma/General Surgery, 1 in Anesthesia, 1 in Psychiatry, 1 in OB/GYN, 1 in Orthopedics, and 1 in Pediatric Emergency Medicine at SickKids. The number of EM blocks completed is dependent on their Goal Directed Experiences (GDE). The GDE replaces the traditional “electives”. You can see that it is included in the Master Rotation Schedule More details will be provided about the GDE at a later date.
- GDE request form (Updated May 2020)
Each Rotation has a specific Rotation Plan. Residents should review the Rotation Plans prior to the start of each rotation.
- COD Anesthesia
- COD EM - Junior
- COD-EM- Senior
- COD ICU
- COD OB/GYN
- COD Orthopedics
- COD PEM
- COD Psychiatry
- COD Trauma/General Surgery
- COD Advanced Ultrasound
- COD Toxicology
- COD EMS
- COD Peds and Community Anesthesia
- TtP
- Area of Advanced Learning
In the past, residents in our program were provided with 1-year (PGY 4) to pursue an Area of Advanced Learning (AAL). Due to CBD requirements, this has changed to 6-7 months, and the nature of the AAL will depend on progression through the CBD stages. We will provide residents with more details as we monitor progress.
Competence Committee
- Tim Dalseg (Chair)
- Kaif Pardhan (Program Director)
- Jennifer Chu (Assistant Program Director)
- Martin Horak (St. Michaels Hospital Staff)
- Jacqueline Willinsky (University Health Network Staff)
- Dana Phillips (Sunnybrook Health Science Centre Staff)
- Sarah Kilbertus (Sunnybrook Health Science Centre Staff)
- Dennis Cho (University Health Network Staff)
- Sally Bogoch (University Health Network Staff)
They use all the assessments described above (e.g. EPAs, ITARs, exams, Notes to File, etc.), as well as other relevant criteria (e.g. attendance records, emails to the PD), to make decisions. Every resident will be reviewed by the CC at least two times per year. The CC provides their overall assessment and recommendations to the EMRTC and PD. The PD will meet with the resident (after the CC meeting) to review these recommendations.
Non-CBD Residents
Royal College Specialty Training Requirements/Curriculum in EM
Emergency Medicine is the branch of specialty practice that is concerned with the management of the broad spectrum of acute illnesses and injury in all age groups. The Emergency Medicine specialist is foremost a physician who uses highly developed clinical reasoning skills to care for patients with acute and often undifferentiated medical problems, frequently before complete clinical or diagnostic information is available. The specialist Emergency Medicine physician is an academic and community resource, providing leadership in the administration of emergency departments, emergency medical systems and programs, and the conduct of relevant research and education. He/she assumes these roles with the goal of advancing knowledge and improving individual and/or community health outcomes.
Royal College Specialty Training Requirements/Curriculum in EM
Rotations
- 5 Year Sample Rotation Schedule - Non CBD
- Internal Medicine/MedConsult: Report to
- Elective Requests Form
- Rotation Goals and Objectives
Master Rotation Schedule for Non-CBD Residents
Here is a link to the Master Rotation Schedule for all 5 years for Non-CBD Residents. There are 13 rotation blocks in each academic year. A number of rotations are “on service” (i.e. emergency medicine or related rotations such as EMS and Ultrasound), and some are “off service”. Residents will rotate through our core teaching sites, as well as affiliated sites.
Core sites:
- Sunnybrook Health Sciences Centre (SHSC)
- St. Michael’s Hospital (SMH)
- University Health Network (UHN): includes Toronto General Hospital (TGH) and Toronto Western Hospital (TWH)
Affiliated Sites:
- North York General Hospital (NYGH)
- Hospital for Sick Children (HSC)
Internal Medicine/Medical Consult Rotation:
Rotation Request Form
Each year, around February, Residents will be contacted by the Program Administrator to submit a Rotation Request Form (updated Spring 2020) for their rotations for the next academic year. The program will try an accommodate requests where possible.
Elective Requests
When choosing an elective that is not arranged by the programs, Residents must complete the “Elective Request Form” and submit this form to the program for approval. Upon receiving approval, the program will provide a paper evaluation (ITER) to the resident for their elective supervisor to complete at the end of the rotation. The resident can then confirm their elective rotation with the rotation site.
Rotation Goals and Objectives
The Rotation Goals and Objectives are reviewed annually. This includes Rotation Goals and Objectives for Emergency and Off-Service Rotations for Emergency Medicine Residents.
PGY4 Area of Advanced Learning/ Subspecialty
The University of Toronto provides an opportunity for a non-CBD PGY 4 advanced area of learning (AAL) year, in which each resident personally designs an AAL curriculum. This curriculum must abide with the Royal College Emergency Medicine committee requirements and be submitted to and approved by the EMRTC during the PGY 3 year. Residents should review the Subspecialty Policy gain clarity and guidance regarding the requirements for the AAL year.
Residents will be asked to fill out the Subspecialty Form in the early fall of their PGY3 year.
In the past, areas of focus have included: pediatric emergency medicine; Masters of Clinical Epidemiology; Masters of Medical Education; Masters in Health Administration; inner city health; international health; toxicology; trauma; critical care medicine; sports medicine; prehospital care; medical informatics; research; aeromedical transport; clinician-scientist program; bioethics; international emergency medicine; ultrasound; simulation, and geriatric emergency medicine.
Resident Rounds/ Learning Opportunities
Our program has one full academic day per week (Wednesday). Attendance at the academic day (both morning and afternoons) is mandatory.
Attendance Policy
Please refer to this document for the full attendance policy
Please review scheduled session on our Google calendar. We recommend you sync this calendar with your own ical or Google calendar, so changes will be reflected in your own calendars.
Afternoon Sessions - Longitudinal Curriculums
There are a number of longitudinal academic day sessions that are provided to our residents at different stages of residency:
Full description is found here
- Journal Club – all years
- Wellness Rounds – all years
- Simulation – all years (note: a separate schedule is sent for simulation so you will know which sessions you need to attend)
- Leadership and Advocacy Rounds – all years
- Clinical Epidemiology and sessions on Foundations of developing a Resident Academic Project – end of PGY 1
- Ethics – PGY 2
- Quality Improvement – PGY 2, 3, 5
- Geriatrics – PGY 3
- Administration – PGY 5
Please review the calendar event details to ensure you attend the sessions which apply to your year.
Feedback & Assessments
Power Evaluations
In-Training Exams
You are required to attend mock orals and written exams as scheduled by the Program